Inter- and Intra- Rater Reliability of Navicular Drop Tests Position
© 2019 by the Korean Physical Therapy Science
Abstract
Pes planus, or flat foot, causes lower limb malalignment and foot pain during walking or exercise. Therefore, a highly reliable evaluation method to accurately diagnose flat feet is necessary. This study investigated the intra-and inter-rater reliability of the navicular drop test in different postures.
Cross sectional study.
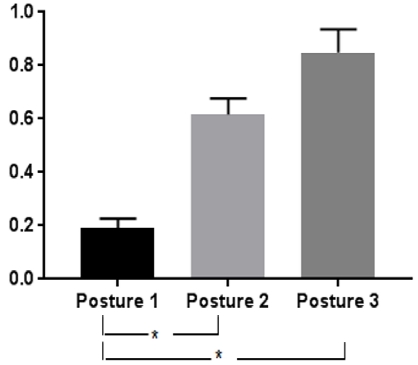
Forty healthy volunteers performed the navicular drop test in three different combinations of non-weight-bearing and weight-bearing postures (standing/standing, sitting/sitting, and sitting/standing). Two examiners alternately performed the measurements five times in each subject, and in each posture. Significant differences in measurements were obtained among the three postures, with the highest navicular drop being observed in the sitting/standing posture.
Inter-rater reliability was high in the sitting/standing and sitting/sitting postures. Intra-rater reliability was high in all three postures. In the sitting/sitting and sitting/standing postures, large navicular drop values and high inter- and intra-rater reliability were observed.
Therefore, the sitting/standing and sitting/sitting postures are recommended for use in navicular drop tests to diagnose flat feet.
Keywords:
Flat foot, navicular drop test, pes planusⅠ. Introduction
In flexible flat feet, the inner vertical arch appears normal when not bearing weight, but collapses excessively on weight bearing (Neumann DA, 2013). This condition is caused by the inability to maintain the medial longitudinal arch due to excessive extension of the plantar fasciitis and dysfunction of the tibialis posterior, leading to excessive pronation of the subtalar joint. As a result, the affected person experiences pain in the tibialis anterior and the gastrocnemius, foot fatigue associated with tingling and numbness, and frequent foot pain during walking and exercise (Harris EJ et al, 2004; Wang W, 2004). These bottom-up phenomena induce pain due to malalignment of the entire lower limb.
Pedobarography and the navicular drop test can be used to diagnose flexible flat feet (Lee TH et al, 2016). The utility of pedobarography is limited because it is time-consuming, expensive, and requires space for electronic equipment to measure foot pressure. In contrast, height differences in the navicular bone between non-weight-bearing and weight-bearing postures can be easily measured and compared by the navicular drop test (Mueller MJ et al, 1993). Therefore, the navicular drop test is commonly used in clinical practice and is associated with no space or cost limitations. The criterion for a flat foot is navicular drop ≥ 0.8 mm, where this measurement is likely to be affected to some degree by the examiner or measurement posture (Vicenzino B et al, 2005; Eom JR et al, 2014; Boergers R, 2000). Identification of the position of the navicular bone and measurement of its height are performed by the examiner, and may be subject to intra- or inter-rater variability. In addition, differences in the amount of weight applied to the navicular bone between non-weight-bearing and weight-bearing postures may affect the height of the navicular bone. Therefore, it is necessary to investigate the effect of various postures on measurements obtained in the navicular drop test, and on its intra- and inter-rater reliability, to determine the most accurate method for diagnosing flexible flat feet.
Ⅱ. Method
1. Participants
Forty healthy college students voluntarily participated in this study. Eligibility criteria included no leg or ankle treatment during the 6 months prior to the study and no musculoskeletal or neurological disorders. The subjects were provided with a sufficient explanation of the purpose and methods of the experiments, and written consent for voluntary participation in the study was obtained <Table 1>.
2. Navicular drop test
The navicular test was conducted using three different combinations of non-weight-bearing and weight-bearing postures. The difference between the height of the navicular bone during weight-bearing and its non-weight-bearing height was defined as the navicular drop.
The first posture tested was the standing/standing posture, in which the height of the navicular bone was measured while the subject applied weight equally to both legs in a standing position (non-weight-bearing), and again while the subject applied weight to the leg to be measured in a standing position (weight-bearing) (Figure 1).
The second posture tested was the sitting/sitting posture, in which the height of the navicular bone was measured while the subject did not apply weight to either leg in a sitting position (non-weight-bearing), and again while the subject applied weight to the leg to be measured in a sitting position (weight-bearing) (Figure 2).
The third posture tested was the sitting/standing posture, in which the height of the navicular bone was measured while the subject did not apply weight to either leg in a sitting position (non-weight-bearing), and again while the subject applied weight to the leg to be measured in a standing position (weight-bearing) (Figure 3).
3. Procedure
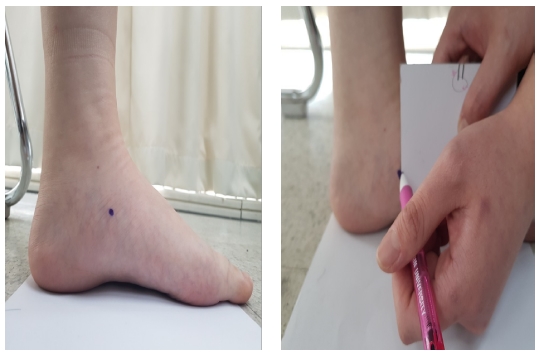
When the height of the navicular bone was measured, its position was marked by the first examiner on the part of the navicular tuberosity showing the greatest protrusion in the horizontal plane using a water-based marker (a); the mark was then removed to conceal it from the second examiner (b). To measure the height of the navicular bone, a large piece of cardboard was placed perpendicular to the ground; the distance between the ground and the navicular tuberosity was marked on the cardboard, and then measured with a ruler (Figure 4). Two examiners conducted measurements alternately, and the readings were reported separately to a data-recording participant, such that each examiner was blind to the other examiner’s results. Measurements were conducted five times in each position, and the maximum and minimum values were removed from the analyses. A 5-min break was provided between postures.
4. Statistical Analysis
All analyses were performed using SPSS software (ver. 20.0; SPSS Inc., Chicago, IL, USA). Navicular drop measurements in the three postures were compared by one-way analysis of variance (ANOVA). Intra-and inter- rater reliability was assessed based on the intraclass correlation coefficient (ICC [2,1]). Significance was taken as P < 0.05.
Ⅲ. Result
Significant differences in navicular drop were found among the three postures, being greatest in the sitting/standing posture (0.84 ± 0.02 cm) (Figure 5). The inter-rater reliability ICC was very high for the sitting/standing (0.841) and sitting/sitting postures (0.735). The intra-rater reliability ICC was very high for all three postures (standing/standing, 0.738; sitting/sitting, 0.911; sitting/standing, 0.937) <Table 2>.
Ⅳ. Discussion
Significant differences were detected among all three postures during navicular drop measurements. The navicular drop values were in the following order: standing/standing > sitting/sitting > sitting/standing. This result can be explained by the fact that, in the standing position, the foot to be measured bore some weight even in the non-weight-bearing posture, such that the difference in navicular bone height between the non-weight-bearing posture and the weight-bearing posture was small. No weight was applied in the sitting/sitting or sitting/standing non-weight-bearing postures. however, in the weight-bearing posture, the difference in navicular bone height appeared to be larger between the standing position, when the entire body weight was applied to the foot to be measured, and the sitting position, when only upper body weight was applied to the foot. The sitting/standing posture is that most commonly used in navicular drop tests, where previous studies have reported navicular drop values as large as 1 cm (Eom JR et al., 2014; Kim TH et al, 2011; Del Rossi G et al, 2004; Ki JW et al, 2010). Therefore, conducting the navicular drop test in the sitting/standing posture is expected to provide a more accurate diagnosis of flexible flat feet than the other postures examined in this study.
Intra- and inter-rater reliability scores were high for the sitting/sitting and sitting/standing postures, but low for the standing/standing posture (McPoil TG et al, 2008). This is likely due to the weight distribution of the subject during the non-weight-bearing part of the standing/standing posture causing differences in the navicular bone height. Therefore, due to examiner inconsistency, the standing/standing posture is not recommended for the navicular drop test.
The high reliability for the sitting/sitting and sitting/standing postures was likely due to the accuracy of the measurement method. In the typical method, the distance from the ground to the lowest part of the navicular bone is measured using a ruler and digital calipers (Vicenzino B et al, 2005; Eom JR et al, 2014; Kim TH et al, 2011). Under such circumstances, it is difficult to precisely position the zero point of the ruler on the floor and maintain the ruler in a truly vertical position. In the current study, the navicular tuberosity was marked at the highest point from the horizontal plane; instead of then determining the distance between the ground and the mark by direct measurement with a ruler, this distance was marked on a piece of cardboard, eliminating the difficulties associated with ruler placement. Therefore, our method improved the accuracy of navicular drop measurements.
Ⅴ. Conclusion
In this study, navicular drop measurement accuracy, and the intra- and inter-rater reliability of the navicular drop test, were compared among three postures. The measurement accuracy and reliability were high in the sitting/sitting and sitting/standing postures. Therefore, these two postures are recommended for navicular drop test measurements, to improve the accuracy of flexible flat foot diagnosis.
Reference
- Boergers R. Effect of arch taping on peak force, contact surface area and neuromuscular activity at midstance.University of Winsconsin-LA Crosse. 2000.
-
Del Rossi G, Fiolkowski P, Horodyski MB et al. For how long do temporary techniques maintain the height of the medial longitudinal arch? Phy Ther Sport. 2004;5(2):84-9.
[https://doi.org/10.1016/j.ptsp.2004.02.001]

-
Eom JR, Moon DC, Kim JS. The changes of balance performance by low-dye taping application on flexible flatfoot. J Korean Soc Phy Med. 2014;9(4):355-61.
[https://doi.org/10.13066/kspm.2014.9.4.355]

-
Harris EJ, Vanore JV, Thomas JL et al. Diagnosis and treatment of pediatric flatfoot. J Foot Ankle Surg. 2004;43(6):341-73.
[https://doi.org/10.1053/j.jfas.2004.09.013]

- Ki JW, Lee EH, Ko KH et al. The effects of navicular drop on the clinical measures of lower extremity alignment. Korean J Orthop Manu Ther. 2010;16(1):1-8.
- Kim TH, Koh EK, Jung DY. The effect of arch support taping on plantar pressure and navicular drop height in subject with excessive pronated foot during 6 weeks. J Korean Soc Phy Med. 2011;6(4).
-
Lee TH, Chay SW, Kim HJ. Diagnosis of flat foot. J Korean Foot Ankle Soc. 2016; 20(1).
[https://doi.org/10.14193/jkfas.2016.20.1.1]

-
McPoil TG, Cornwall MW, Medoff L et al. Arch height change during sit-to-stand: An alternative for the navicular drop test. J foot Ankle Res. 2008;1(1):3.
[https://doi.org/10.1186/1757-1146-1-3]

-
Mueller MJ, Host JV, Norton BJ. Navicular drop as a composite measure of excessive pronation. J Am Podiatr Med Assoc. 1993;83(4):198-202.
[https://doi.org/10.7547/87507315-83-4-198]

- Neumann DA. Kinesiology of the Musculoskeletal System-E-Book: Foundations for Rehabilitation. Elsevier Health Sciences, 2013.
-
Vicenzino B, Franettovich M, McPoil T et al. Initial effects of anti-pronation tape on the medial longitudinal arch during walking and running. Br J Sports Med. 2005;39(12):939,43; discussion 943.
[https://doi.org/10.1136/bjsm.2005.019158]

-
Wang W, Crompton R. Analysis of the human and ape foot during bipedal standing with implications for the evolution of the foot. J Biomech. 2004;37(12):1831-6.
[https://doi.org/10.1016/j.jbiomech.2004.02.036]